R Lobectomy
Posted : admin On 3/18/2022| Anterior temporal lobectomy | |
|---|---|
| ICD-9-CM | 01.53 |
| MeSH | D038481 |
R Nephrectomy

- Thoracoscopic lobectomy is designed to achieve the same oncologic result as conventional lobectomy: complete hilar dissection and individual vessel control. The recognized advantages of thoracoscopic anatomic resection include less short-term postoperative pain, shorter hospital stay, and preserved pulmonary function.
- Each of your lungs is made up of sections called lobes. The right lung has three lobes, and the left lung has two. A lobectomy is a type of lung cancer surgery in which one lobe of a lung is removed because it contains malignant tumors.
R/LobotomyCorp: Welcome to the Lobotomy Corporation subreddit! Monster Management, Rogue-Lite Simulation game, where you contain different. Lobectomy has been the standard of care for patients with stage I primary non-small cell lung cancer (NSCLC). Historically, this is based on the results of the Lung Cancer Study Group (LCSG) trial reported by Ginsberg and Rubinstein. Life After Lobectomy: 6 Steps to a Smooth Recovery After Lung Cancer Surgery. Returning to regular life at home after lung cancer surgery can be daunting.
Anterior temporal lobectomy is the complete removal of the anterior portion of the temporal lobe of the brain. It is a treatment option in temporal lobe epilepsy for those in whom anticonvulsant medications do not control epileptic seizures.
The techniques for removing temporal lobe tissue vary from resection of large amounts of tissue, including lateral temporal cortex along with medial structures, to more restricted anterior temporal lobectomy (ATL) to more restricted removal of only the medial structures (selective amygdalohippocampectomy, SAH).
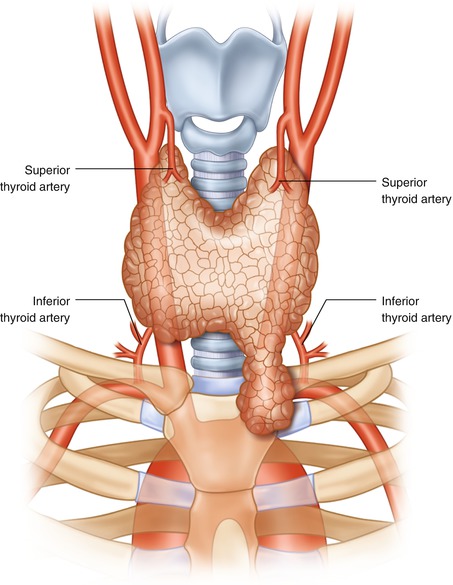
R Thyroid Lobectomy
Nearly all reports of seizure outcome following these procedures indicate that the best outcome group includes patients with MRI evidence of mesial temporal sclerosis (hippocampal atrophy with increased T-2 signal.) The range of seizure-free outcomes for these patients is reported to be between 80 and 90%, which is typically reported as a sub-set of data within a larger surgical series.[1][2]
Open surgical procedures such as ATL have inherent risks including damage to the brain (either directly or indirectly by injury to important blood vessels), bleeding (which can require re-operation), blood loss (which can require transfusion), and infection. Furthermore, open procedures require several days of care in the hospital including at least one night in an intensive care unit. Although such treatment can be costly, multiple studies have demonstrated that ATL in patients who have failed at least two anticonvulsant drug trials (thereby meeting the criteria for medically intractable temporal lobe epilepsy) has lower mortality, lower morbidity and lower long-term cost in comparison with continued medical therapy without surgical intervention.
What To Expect After Lobectomy

The strongest evidence supporting ATL over continued medical therapy for medically refractory temporal lobe epilepsy is a prospective, randomized trial of ATL compared to best medical therapy (anticonvulsants), which convincingly demonstrated that the seizure-free rate after surgery was ~ 60% as compared to only 8% for the medicine only group.[3] Furthermore, there was no mortality in the surgery group, while there was seizure-related mortality in the medical therapy group. Therefore, ATL is considered the standard of care for patients with medically intractable mesial temporal lobe epilepsy.
References[edit]
R Thoracotomy Procedure
- ^Engel J (March 1996). 'Surgery for seizures'. The New England Journal of Medicine. 334 (10): 647–52. doi:10.1056/nejm199603073341008. PMID8592530.
- ^Spencer SS, Berg AT, Vickrey BG, Sperling MR, Bazil CW, Shinnar S, Langfitt JT, Walczak TS, Pacia SV (September 2005). 'Predicting long-term seizure outcome after resective epilepsy surgery: the multicenter study'. Neurology. 65 (6): 912–8. doi:10.1212/01.wnl.0000176055.45774.71. PMID16186534.
- ^Wiebe S, Blume WT, Girvin JP, Eliasziw M (August 2001). 'A randomized, controlled trial of surgery for temporal-lobe epilepsy'. The New England Journal of Medicine. 345 (5): 311–8. doi:10.1056/NEJM200108023450501. PMID11484687.
Upper Right Lobe Removal
External links[edit]
